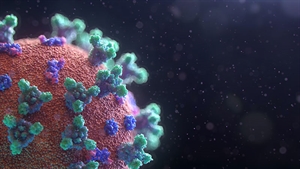
Covid-19 (Novel Coronavirus-19) is an infectious disease which is contagious and has not been previously identified in humans. It was first found in Wuhan, China in December, 2019 from where it spread all over the globe. On 30th January, 2020, the World Health Organization declared the coronavirus outbreak a public health emergency of international concern, and on 11th March 2020, declared it a pandemic. The disease is rarely fatal. It primarily attacks people with weak immunity. This mainly includes old people as well as people with pre-existing respiratory, lung or heart diseases and diabetes. As of 18th April, 2020, 2.25 million cases have been reported across the globe. 571,000 people have recovered where as more than 154,000 deaths have occurred. There is no definite treatment for covid-19, as of yet. Extensive research is being held by scientists in regard to a safe and effective treatment. Currently, pre-existing drugs and anti-virals that were developed for other diseases and viruses are being used to relieve the symptoms.
How far are we from Covid-19 Vaccine?
The difference between drugs and vaccines should be understood. Drugs are used to treat disease and viruses whereas vaccines are used to prevent them. Covid-19 is being treated using drugs but there is no specific treatment for it as of yet, as mentioned earlier. As you would assume, there is no vaccine for covid-19 as well. Experts have estimated that a vaccine for covid-19 could take anywhere from a year to 18 months, maybe more, to be developed, approved and ready for use for the public.
Vaccines and drugs have to be tested in laboratories and on animals, after which they have to undergo several clinical trial stages, to ensure that they are safe to use. This is also to estimate the dosage required. Scientists also have to make sure a sufficient number of people are included in each stage, which is why it takes a long time to develop vaccines and cannot be sped up. They also have to wait for an appropriate amount of time to check for harmful after effects.
In the first stage, the drug is tested on a small number of people, some healthy and some infected, to see the response and figure out the best dosage. In the next stage, the drug is given to a slightly larger group of people, typically ranging from 100-300 people. In this stage, the purpose is to look for any side effects that were not caught in the previous stage. If the drug shows an excellent response in bettering immunity, it reaches third stage where it is given to a large number of people, a several hundred or even thousands. This stage is the most crucial as it gives the most accurate results of the workings of the drug and side effects. If the drug gets approved, it is then tested continually to make sure there are no serious or long-term harmful effects. Each of these stages can take 3 to 6 months. The third stage can even take up to a year or several years.
According to the World Health Organization, over 70 different vaccines are in development worldwide. Many of these have begun clinical trials on human beings who have volunteered. Due to the rapid spread of the disease and the urgency to slow it down and lessen the damage, researchers are working tirelessly to speed up the processes. There are several approaches being adopted for the development of the vaccine for covid-19 by different countries and their institutions.
Sarah Gilbert, Professor of Vaccinology at the University of Oxford and top scientist at the university’s Jenner Institute, along with her research team started investigating and researching covid-19 in the early days of 2020. Once the scientists in China released the genome sequence of Sars-CoV-2 – the virus that causes the disease, Gilbert and team set out to develop a vaccine for covid-19 and dedicated all their efforts towards it. U.K.’s National Institute for Health Research and the UK Research and Innovation awarded a 2.2 million-pound ($2.8 million) grant to Gilbert to make progress with the vaccine and move it into the clinical trial stages, being the first to do so. Gilbert’s colleague, Sandy Douglas’s vaccine manufacturing also received funding alongside her. She talked about the importance of funding and acknowledging the different aspects leading to the vaccination developments and then the stages after and how it is important to work side by side in these trying times.
500 people have volunteered ranging from the ages 18-55 to be the subjects of the first clinical testing. Gilberts hopes to have them successfully vaccinated by mid-May. The next step would be to increase the age range and bring it up 18-70 and later extending the limit to 75. Stage 3 of the clinical trial is expected to enroll 5000 volunteers. Gilbert claims that she is 80% positive that the vaccination will work, as it uses the same base model which has been previously used for the vaccines that she and her team progressed work on, such as Influenza and Zika virus and early stage trials for Middle East respiratory syndrome coronavirus vaccine. “The best-case scenario is that by the autumn of 2020, we have an efficacy result from phase 3 and the ability to manufacture large amounts of the vaccine, but these best-case timeframes are highly ambitious and subject to change”, Gilbert says, in an interview.
The World Health Organization is arranging a platform for all the different research teams across the world to come together and share information and findings amongst each other to boost knowledge and the pace of progress. This will also allow everyone to speed up the clinical trial process as tests can be held parallel to each other and manufacturing can be initiated side by side as well.
The first vaccine in the US to move into clinical trials is developed by Moderna, a biotech firm. The firm recruited 45 healthy volunteers all aged 18-55 in Seattle, Washington to be tested for the experimental covid-19 vaccine. The volunteers will be divided into three groups and will be given different doses to figure out the best dosage along with any side effects. Moderna was able to skip pre clinical stages like animal and lab testing as their vaccine does not have the virus that triggers the disease. Instead, it uses RNA, or mRNA, which is a genetic material that is produced in a lab. After the initial testing, the vaccine will be distributed and tested in larger groups of people.
Inovio Pharmaceuticals was working on DNA vaccines for MERS in late 2019 so when covid-19 surfaced, Inovio developed a potential vaccine for it which was approved by the US Food and Drug Administration (FDA). They have been successful in preclinical trials and have proceeded onto phase 1 of clinical trials on 40 healthy individuals from the University of Pennsylvania and Center for Pharmaceutical Research in the US. They have already produced thousands of INO-4800 doses for clinical trials and plan to produce a million doses by the end of 2020 for further trials and emergency use. They have also been granted a $6.9million funding by Coalition for Epidemic Preparedness Innovations (CEPI) to work with South Korea based International Vaccine Institute (IVI) and the Korea National Institute of Health (KNIH) for phase 1 and 2 clinic trials of Inovio’s candidate vaccine for covid-19.
Dow University of Health Sciences in Karachi, Pakistan has prepared intravenous immunoglobulin (IVIG) with plasma that is obtained from the blood of patients that have recovered from covid-19. It has to be acknowledged that this method is different from plasma therapy which is only allowed in severe emergencies due to its side effects, whereas IVIG treatment is approved by the US Food and Drug Administration (FDA) under normal circumstances. This method is safe and highly effective along with very little risks as it uses purified antibodies instead of the whole plasma and does not carry unwanted blood components. IVIG treatment has proved successful in laboratory testing and safety trial on animals and is moving onto clinical trials on humans. The team is working to scale-up the production process and collecting more and more blood donations. Six renowned multinationals companies are following Dow University’s lead for IVIG treatment and are highly positive that it is a major break-through in the fight against covid-19.
Even if a vaccine for covid-19 emerges soon and successfully, and is able to be given to the masses, it is possible that it could wear off in a couple of years. It is possible that these accelerated vaccine development processes and shortcuts could impact the efficacy of the vaccines and the search for the best vaccine might still continue in the coming years if covid-19 turns into an epidemic, which is highly likely.
Andino-Pavlovsky, Professor in the Department of Microbiology and Immunology at the University of California, said that extensive research should be continued for coronavirus immunity even after a vaccine is developed, “not only for COVID-19, but for the next coronavirus that comes.”